Gert Galster
Medical Informatics Group, Department of Health Science and Technology, Aalborg University, Aalborg, Denmark
Abstract
There is a widespread health informatics vision of unlimited exchange, understanding and reuse of clinical information. However, it has also been pointed out that to understand clinical information it is to some extent necessary to know the circumstances of its production - the production-contextual clinical information.
The purpose of this study was to investigate the nature and significance of production-contextual clinical information in doctors' everyday clinical work in order to asses whether standardization is necessary and possible. The study was performed through observation and focus group interviews at a cardiology department in a midsize Danish hospital.
It was found that production-contextual clinical information is complex, extensive, non-quantitative, and that it has an elusive structure. It is concluded that while it may be possible to standardise a limited amount of production-contextual clinical information, a general standardisation may very well be impossible.
Keywords
Medical informatics, Electronic health records, Clinical information, Context
1 Introduction
Over several years, there has throughout the health informatics community been a widespread common vision of universal interoperability. The vision has been described numerous times, e.g. in the Semantic Health Report[1] which sketches a scenario where health-related information can be shared seamlessly across national boundaries, where clinical information can be exchanged and reused for both clinical and non-clinical purposes, and where any health actor can understand and integrate the information in a collaborative manner as if the information was generated locally. A key element towards this vision is the systematic standardisation of information that is essential to everyday clinical work.
On the other hand, it has been pointed out that both primary and secondary utilisation of health information can be critically dependent on production-contextual clinical information, i.e. the description of the circumstances of obtaining clinical information[2][3]. It has also been described that standardisation of contextual information poses several problems - not the least to delimit context, and to formalise it[4][5][6][7]. Thus, the need for standardisation of production-contextual information has the potential to be a major obstacle to the realisation of the envisioned degree of interoperability.
The objective of this study was to investigate the nature and significance of production-contextual clinical information in the everyday clinical work of physicians in order to assess whether standardisation is necessary and possible. Thus, the study should answer these three questions:
- What constitutes production-contextual clinical information?
- What is production-contextual clinical information used for, and to what extent does it impact on everyday clinical work?
- How can production-contextual clinical information be operationalized in order to support clinical reasoning?
1.1 The Perception and Significance of Context
This study's overall perception of 'context' is based on the definition given in ISO/TR 17119:2005 Health informatics profiling framework:
related conditions and situations that provide a useful understanding and meaning of a subject[8]
As pointed out by Winograd[5] and Dourish[6], context can be viewed as fixed and pre-determined, or as variable and situational. In this project, context is perceived as highly situational. As expressed by Winograd:
Context is an operational term: Something is context because of the way it is used in interpretation, not due to its inherent properties[5].
Thus, rather than perceiving context as something which can be designated in advance, this study is based on the perception that context is what a given actor in a given situation considers of relevance. Furthermore, contextual information is perceived as a description of context for the purpose of communication.
But even though information is described as relevant, it may be more or less significant. It has been exemplified that contextual clinical information may be of crucial importance[2][3][9], but it is not clear to what extent this is true in everyday clinical work. For the sake of operationality, this study perceives contextual clinical information as essential, if it by inference leads to explicit reconsideration of existing information.
1.2 Contextual Clinical Information
Communication based on documented clinical information (e.g. progress notes, lab results) is one-way, and not real-time. It is thus possible to view communication through a simple model with a sender and an unknown number of receivers where sender has a very limited knowledge, if any, of the receiver(s).
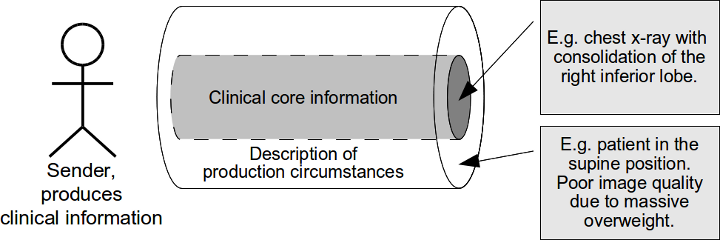
Fig. 1. Production-contextual clinical information
With reference to Fig. 1: Health information is produced under some circumstances and documented by the sender as a core of clinical information. A description of the circumstances may be documented along with the core. E.g. a radiologist describes a chest x-ray with (as core information) consolidation of the right inferior lobe. He mentions (as a description of production circumstances) that the patient was in the supine position, and that the image quality is poor due to massive overweight.
At a later time, a receiver reads the documentation. In order to achieve a useful understanding and meaning of the message core, the receiver needs to understand the former circumstances.
Thus, production-contextual information is not a description of what the sender considered relevant in the situation, but of those details of the sender's situation which the receiver finds of current relevance.
2 Materials and Methods
Doctors' use of production-contextual clinical information was studied through observations and focus group interviews. The basic question posed was which supplementary information the doctors requested, and whether the requested information concerned the circumstances of obtaining information - i.e. whether production-contextual information was requested.
2.1 Observations and Interviews
The observations and interviews were done in the Cardiology Department of Bispebjerg Hospital in Copenhagen - a mid-size hospital in the capital region of Denmark.
Observations were performed at five random morning conferences for doctors. The conferences included two types of scenario: the reporting of yesterday's patients and the collective analysis of selected case stories. The focus of observation was the recurring requests for additional information, and whether the requested information was production-contextual.
The interviews were carried out as five sessions of focus group interviews[10] with three to six doctors in each. As preparation for the interviews, different pieces of clinical information were collected from random cardiology health records. A total of 63 pieces of information were collected. In order to ensure a fair coverage of healthcare activities, the below mentioned analytical framework was used as a guide for selection. Thus, all information types were represented, e.g.
- "Pt. has consented to angioplasty” (Observation)
- "Peripheral venous access was obtained” (Action)
- "Diagnosis: fever with no known cause” (Opinion-Diagnosis)
- "Pt. should lose at least 10 kg” (Opinion-Goal)
- "Plan: observation in telemetry for the next 24 hours” (Instruction)
| Healthcare activity |
Basic information type | Information subtypes |
|---|---|---|
| Observation | Observation |
|
| Action | Action |
|
| Evaluation | Opinion |
Diagnosis Risk Prognosis Scenario Goal Recommendation |
| Instruction | Instruction |
Investigation request Intervention request |
The collected pieces of information were printed out as cards, and used as basis for the interviews as follows: the participants would draw a card at random and use this single piece of information as their focus for discussion. Their objective was to specify which supplementary information they would require, and the significance thereof.
As the need for supplementary information depends on the specific situation, and in order to keep focus on the piece of information at hand, it was decided to avoid any indication of situational context. Hence, the participants had to discuss the significance of requested information for varying situations.
2.2 Analytical Framework
In the present study the generation and usage of clinical information was analysed on the basis of the model described by Beale & Heard[11]. This model describes four kinds of healthcare activities (by implication) and ten corresponding clinical information types, as shown in Table 1.
This framework was used for the collection of information from health records and for the analysis of observations and interviews.
3 Results
3.1 Observations
When observing the flow of information at the doctors morning conferences, it was noticed that every presentation of a new patient began with a "starter package" consisting of the basic observations of age and gender, the diagnoses which were the reason for the current encounter, any relevant co-morbidity, and a statement regarding the status in relation to the current encounter. E.g. "63-year-old female with no history of serious illness is admitted with suspected AMI. Non-specific ECG changes. Coronar enzymes are under way.”
Then supplementary information was presented in a dialogue of questions and answers until some kind of decision or collective perception was reached. The case stories followed the same path, except that the initial narrative was more fluent, and the questions more pointed.
During the five conferences, a total of 206 instances of supplementary clinical information were recorded. Of these were 54 (26%) found to concern the circumstances of obtaining information, i.e. to be production-contextual information. Examples of the requests for production-contextual information are shown in Table 2.
It was repeatedly observed how a question about some detail regarding a healthcare activity led on to further questions with the obvious purpose to perform source criticism, and assess the credibility of information obtained from the healthcare activity. E.g. a question about when an observation was done, led to further questioning about whether the observation was done spontaneously, and what was the reason for the observer to be there at the time, and was the observed event actually foreseeable. Another example: a question about where an examination was performed, led to a discussion about another hospital's reputation, and whether the examination result should be trusted.
Thus, production-contextual information was through this process of source criticism repeatedly causing reconsideration of clinical information, as illustrated in Table 2. It seemed to be a continuous and integral part of the overall information flow between the doctors.
| Information type |
was reconsidered due to production-contextual information, e.g. |
|---|---|
| Observation |
Doctor-patient interaction - "He seemed not at ease so I am not sure whether he told me the truth about his medication.” Organisational location - "The examination wasn't done here, so we can't use the results as basis for a risky intervention.” Topicality (information shelf life) - "But this ECG is more than a week old!” |
| Action |
Competence - "This echocardiography should have been performed by a specialist." Method - "Are you sure she was informed according to our guidelines?" |
| Opinion |
Quality - "Did she mention her confidence in the diagnosis?" Competence - "If the dietician says so, it's true." |
| Instruction |
Logistics - "I would have prescribed sotalol tablets, but we only had sotalol for injection." Consent - "I would have ordered a PCI, but the patient didn't want it." |
Table 2 illustrates types of clinical information which were reconsidered as a result of production-contextual information. E.g. (observation): A junior doctor questioned a patient about his medication and was told that the patient took his medication as prescribed. However, this information was later reconsidered in the light of the patient's condition at the time of questioning.
3.2 Interviews
As mentioned, the interviews were performed with a single piece of clinical information as focus and without any kind of situational framing. The absence of situational context repeatedly raised some discussion about which situations would constitute a relevant context for the current piece of information. These discussions gave rise to a broad palette of contextual information related to the current piece of information. A few participants, however, noted that they would have preferred real case stories and expressed frustration over the absent situational context which made it difficult to relate to the given piece of information.
During the five interviews, the participants requested a total of 67 instances of supplementary clinical information. Of these, 40 instances were found to be production-contextual.
The question on information credibility was a major topic, and even more so than during the observed conferences. The participants repeatedly requested supplementary information in order to perform source criticism, i.e. for balancing of likelihood, credibility, and overall weight of the given information.
From the discussions between the participants on what could be context for a given piece of clinical information, it was evident that they perceived contextuality as highly situational. In addition, the discussions repeatedly touched on significance being situational. Thus, it was again and again pointed out that even if a piece of contextual information, e.g. the description of an operation, in the majority of cases were only of interest as an outline of what had happened, there could be situations where the precise details, e.g. the use of certain materials or implants, would be crucial.
3.3 Data Processing
The outcome of observations and interviews were coded according to the above mentioned analytical framework. It was thus possible to group the (54 + 40= ) 94 instances of production-contextual information according to their related type of healthcare activity, i.e. groups concerning clinical information obtained by observation, action, evaluation, and instruction, see Table 1.
In an attempt to organize the contents of each of the four groups, it became clear that there is no obvious connection between healthcare activity and contextualized clinical information. Hence, it was only possible to make a very general categorisation. Table 3 shows an overall view on the collected production-contextual information organised with the healthcare activity as key and according to the "Kipling method" (5W1H).
|
4 Discussion
4.1 The Use of Production-Contextual Clinical Information
Several authors, e.g. [12], [2], [3], [9], have from examples of production-contextual clinical information deduced that knowledge of the healthcare activities that produce clinical information is essential for the clinical use of this information. It was an objective of this study two investigate whether these examples are rule or exception. In order to operationalize the importance of contextual information, it was assessed against whether it led to explicit reconsideration of existing information. This delimitation, while seemingly arbitrary, reflects a pragmatic choice: firstly, the delimitation is based on actual relevance; secondly, the condition is directly observable.
The observations of doctors' morning conference demonstrated that the participating doctors, based on the clinical information, repeatedly requested information about how the clinical information was produced - i.e. production-contextual clinical information.
Observations for this study were performed at a single department, and it cannot be ruled out that doctors in other circumstances have access to more consistent and unambiguous clinical information. However, the observed amount of significant production-contextual information, and the ease with which the doctors changed plans as a consequence of it, leaves the impression that handling of essential production-contextual information is a continuous and integral part of clinical everyday work.
During the observations, it was noticed that production-contextual clinical information to a great extent was used for source criticism, i.e. for balancing of likelihood, credibility, and overall weight of information concerning the patient. This is consistent with the findings by Kassirer & Gorry[12] who in detail describe several of the underlying mechanisms for critically gathering of clinical information, including the need for, and the comprehensive use of, source criticism in doctor's problem solving.
4.2 The Nature of Production-Contextual Clinical Information
The sample of observed instances of production-contextual clinical information was too small to give an in-depth understanding of what this kind of information consists of. This in itself could explain why the collected production-contextual clinical information was so difficult to categorise, cf. Table 3 . However, from the collected instances it is obvious that they include in considerable degree information that is complex (e.g. education, experience) and qualitative (e.g. mental capacity, intensity of treatment). Besides, several authors, e.g. [4], [5], [6], [7], have pointed out the difficulty of defining and modelling context. As stated by Bricon-Souf&Newman:
One difficulty is, as yet, the research community has not reached a consensus as to the best way to model context and architectures to support its use[7].
Furthermore, it has been pointed out that the interpretation of a single piece of clinical information must take into account
… an in principle interminable list of context attributes, each with a weight determined both by the context in which the piece of information is currently to be used and the context in which it was originally recorded [13].
Basically, production-contextual clinical information is information related to a healthcare activity, and it is therefore not surprising that the description of the activity itself - the who, what, when, where, why, and how - is an essential part of the collected production-contextual clinical information. The material from this study, however, demonstrates that production-contextual clinical information includes far more than just a description of the healthcare activities; e.g. not only the simple "who?", meaning "which patient and which healthcare professionals?", but in addition a diverse amount of derivative information like the patient's spatial orientation, mental capacity, and whether on leave, and the healthcare professionals' education, organizational affiliations and experience. So while the basic who, where, when, and what may be easily obtained from existing structured sources, the basic why and how will probably need some human registration. And the real challenge lies in the need for an ascending order of derivative information like the doctor's experience with this procedure, with this procedure under these circumstances, with this procedure under these circumstances using this technique, and so on.
In this context it should also be noted that while this study registered 94 instances of production-contextual clinical information the actual incidence is necessarily greater. Thus, it was often a matter exactly who had provided the clinical information (e.g. by performing an examination), and since the staff know each other the naming of a person is also an indication of a number of personal characteristics which can be used in balancing the weight and importance of the clinical information. Likewise, the doctors' common knowledge of work flows, procedures and guidelines constitutes a significant amount of production-contextual clinical information.
It is, without doubt, possible to express some amount of production-contextual clinical information in a structured way, but as an overall concept it seems so extensive, so complex, and with such an elusive structure that an exhaustive structuring of production-contextual clinical information seems to be impossible.
4.3 How To Operationalize Production-Contextual Clinical Information
Production-contextual clinical information can be essential to clinical reasoning and its documentation thus is of importance to supporting of clinical work. This applies in particular if the level of ambition is as outlined in the Semantic Health Report where
… any health actor can understand and integrate the information in a collaborative manner as if the information was generated locally[1].
However, achieving this kind of documentation of production-contextual clinical information is problematic for three reasons:
First, production-contextual clinical information is complex, extensive, non-quantitative, and has an elusive structure. As mentioned above it seems unlikely to develop a model that permits a comprehensive expression.
Second, regardless of model, the amount of production-contextual clinical information needed to meet every health actor’s needs is enormous, even compared to the already huge amounts of clinical core information. The amount of information raises several logistic questions, not the least of how the information should be obtained. Since the production-contextual clinical information largely consists of complex and qualitative information it would require manual registration, and as pointed out by Berg & Goorman, the disadvantages of this registration easily exceeds the benefits [2].
Third, even if the level of ambition is reduced it is challenging to bring about the necessary amount of production-contextual clinical information. As stated in the introduction, production-context is not what the sender considered relevant in the situation, but those details of the sender's situation which the receiver finds of current relevance. So unless the sender is told what contextual information to register, there is no guarantee that the existing production-contextual information will suffice.
On this basis, the operationalization of production-contextual clinical information can include standards and agreements which, in consideration of the registration burden, specify what is to be documented and in what detail. Registration of production-contextual clinical information in an amount that satisfies the vision of the Semantic Health Report [1] seems to be an illusion.
5 Conclusion
Production-contextual clinical information is the description of the circumstances of obtaining clinical information. In this paper the nature of production-contextual clinical information and the implications of its use were studied through observations and focus group interviews at a cardiology department in a mid-size hospital.
The circumstances under which clinical information is obtained can be many and very diverse. Accordingly, it was found that production-contextual clinical information is very extensive, complex, and with an elusive structure. It was also demonstrated that production-contextual clinical information is an integral part of doctors' daily work and that it can be crucial for balancing of likelihood, credibility, and overall weight of the given clinical information. Thus, access to production-contextual clinical information is an essential part of supporting the doctors' clinical work.
The potential volume, the complexity and the elusive structure, however, pose a significant barrier to making production-contextual clinical information available on a large scale. It is recommended that the operationalization of production-contextual clinical information is performed through standards and agreements which, in consideration of the registration burden, specify what is to be documented and in what detail.