Gert Galster, MD MI
Department of Health Science and Technology, Aalborg University, Aalborg, Denmark
Abstract
Traditionally health records have a source-oriented structure, as opposed to a clinically logical structure. The aim of the current study is to record and depict the clinically logical information structure build by doctors as part of their contextualisation of clinical information, to compare this structure to that of a given health record, and to asses whether a structural difference may have negative consequences. Eight doctors in a medical department were observed during contextualisation of clinical information. The method of observation included simultaneously interview and with the technique used it was possible to depict the clinically logical information structure and compare it to the structure of the health record. The doctors' information structure was found to differ widely from the structure of the health record, causing split-attention and stress. It is concluded that the present health record is suboptimal. Further research in information support based on clinically logical structure is recommended.
Keywords
Medical Informatics, Health Information Management, Medical Records, Clinical Information, Clinically logical information structure, Context
Introduction
In the Capital Region of Denmark the transition from a paper-based to an electronic health record has been ongoing for several years. The health record can now be described as source-oriented and highly fragmented[1]. The fragmentation is not necessarily problematic, but if the health record's structure or functionality is not tailored to doctors' needs this can lead to impediments and work flow interruptions[2].
An essential part of the doctors' interaction with the health record is to retrieve information. The inspiration for this study was the finding that pieces of clinical information which from a clinical point of view are closely related must be assembled from various parts of the health record. Thus, it was appropriate to examine to what extent the structure of the current health record supports the doctors' retrieval of information. In the hope to improve the structure of the health record used in the Capital Region of Denmark, this study should answer two questions:
- Is it possible to describe a "clinically logical information structure", meaning a doctor's structuring of clinical information about a specific patient?
- Is a difference in information structuring between doctor and health record likely to have negative consequences for doctors' daily work?
This study concerns a given health record's ability to support doctors' contextualization of clinical information as it manifests itself in their gathering of clinical data. Unlike studies focusing on doctors' cognitive processes and mental work-flow, the topic of this study is not to investigate doctors' varying methods of making clinical decisions[3], neither their methods of data-gathering[4].
A number of terms concerning information systems and information structure are used consistently throughout this paper:
- Electronic health record: The collection of recorded clinical information that is locally available in digital form and concerns a single patient
- Paper-based health record: The collection of recorded clinical information that is locally available in hard copy and concerns a single patient
- Combined health record (or just "health record"): The exhaustive collection of recorded clinical information that is locally available and concerns a single patient.
- Source-section: The general building block of source-oriented documentation, whether digital or paper-based, e.g. lab-results, progress notes, etc.
The perception of contextual information in this paper is based on the work by Winograd[5] and Dourish[6] which describe context in a phenomenological frame as a relational property that holds between objects or activities, and as such is highly situational. Accordingly, this paper is based on the perception that contextual information is information that by a given actor in a given situation is seen as relevant. In this light the retrieving of relevant clinical information is perceived as the manifestation of a contextualization process - an interpretation consistent with Patel et al.’s description of doctors building a clinical context through data gathering[4].
1. Methods and Materials
1.1. Obser-view, Focal Points, and Information Structure
Patel et al.[4] have in detail described doctors' methods of data gathering and how doctors successively build and subsequently use a complete clinical context. The structure of this contextual clinical information, though, has seemingly not been investigated. In order to depict the doctors' clinically logical information structure it was decided to use a think-aloud method as described by e.g. Kushniruk et al. [7], but with a more active prompting. Thus, the empirical material for this work was collected through a method which can be described as observations supplemented by simultaneous interviews. The method has been called obser-view by Kragelund[8] who describes it as a dialogue between research participant and researcher in which they, as a continuation of the researcher’s observation, reflect on the observations made. Hertzum et al. describe the relaxed application of thinking aloud as a method where the participant is urged to describe aspects of the current task in such a detail that it influences the participant’s focus of attention in ways beyond those occasioned by task performance[9]. The obser-view goes even further, in that the participant is actively engaged in dialogue about reasoning and choices made.
The doctor's focus of attention changes between different topics while contextualizing clinical information. The video-supported obser-view made it possible to register these changes as a sequential series of focal points where each focal point represents a distinct topic as expressed by the doctor, e.g. a diagnosis, an organ system, a lab result. In the analysis of the video data, each focal point was registered with the time-stamp, the topic, and the current source-section of the combined health record. The topics were subsequently assembled by the author along the indications from the obser-view. The resulting information structure was depicted in a mind-map (see example in Figure 1). Such a structure is throughout this paper perceived as a doctor's clinically logical information structure concerning a specific patient.
1.2. Hospital, Health Record, and the Participating Doctors
The study was carried out at the medical department at Frederiksberg Hospital – a 700-bed hospital in the Capital Region of Denmark. The health record used there has been under development for several years and is currently based on both digital and paper-based information. Bansler et al.[1] and Nøhr et al.[10] have described the health record from this region as being distributed over an assortment of paper-based and electronic archives and databases and with the content structured according to the method by which it is obtained. Accordingly, the health record in the present study consisted of several source-sections - some digital (e.g. medication list, biochemistry lab results), some paper-based (e.g. ECG, nursing record), and some both (e.g. progress notes, microbiology lab results).
Eight experienced doctors were followed on their ward rounds. In order to investigate how the health record supports the doctors' contextualization of clinical information, a specific task was chosen as the subject of observation, namely the experienced doctor's first review of a newly admitted patient. This task is performed on a daily basis, it includes extensive contextualization, and thus involves the selection and retrieval of a variety of clinical information. The participating doctors were aware that the objective was to uncover their way to find and gather the necessary clinical information. They were prompted to think aloud and to explain what they did. All obser-views were recorded on video. The overall empirical material consisted of 10 hours of recorded obser-view where the eight doctors rounded on 33 patients.
2. Results
2.1. Contextualization
All participating doctors performed the chosen task in the same manner: The doctor read the basic information from the electronic board, retrieved the paper-based health record, logged on to the electronic health record, and performed a comprehensive review of the various source-sections. After a dialogue with the responsible nurse, the patient was interviewed and a physical examination was performed. If needed, the doctor did a supplemental review of various source-sections. Finally, decisions were communicated to the nurse, documented as necessary, and a progress note was dictated. The process was in general performed one source-section at a time. Even though time measurement was not a part of this study, it was noted that switching between digital source-sections was time-consuming. Furthermore, it was repeatedly observed that the shift between digital sections gave rise to idle time and stress.
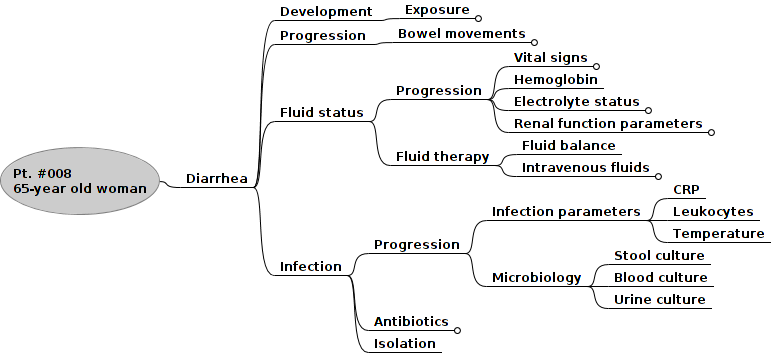
Figure 1. A doctor's clinically logical information structure concerning a 65-year old woman admitted because of diarrhea with onset one week after return from holiday in Italy. Otherwise healthy and with no relevant history. Due to restrictions on figure size, several nodes (e.g. Exposure, Bowel movements) are shown collapsed. The total number of leaf-nodes for this obser-view was 26.
During the doctor's contextualization of clinical information, the obser-view method made it possible to register a sequence of focal points, i.e. a sequence of clinical topics associated with the corresponding part of the health record. On analyzing these sequences, it was for every patient noted how topics were repeatedly postponed. Some doctors kept the varying focal points in memory, while others kept a hand-written running list of focal points that needed further clarification. A few times, not surprisingly, topics were simply forgotten.
The registered focal points can be assembled to a mind-map depicting the doctor's clinically logical information structure, see Figure 1. Every leaf-node and most of the branches are topics expressed by the doctor as focal points. Every obser-view resulted in a unique information structure. There were, however, focal points (e.g. infection, ventilation) where the structure was (almost) identical.
2.2. Comparison of Information Structures
The registration of focal points as associations between clinical topics and source-sections makes it possible to depict how the health record's different source-sections contribute to the contextualization of topics. Figure 2 depicts for a given obser-view the connection between (horizontally) the source-oriented health record's structure, and (vertically) the clinically logical information structure build by the doctor. The bullets identify where information was gathered and to what extent. E.g. all information about exposure was found in the progress notes, while information about infection was gathered from electronic board, progress notes, medication list, microbiology lab results, biochemistry lab results, and nurse documentation.
This example, which is typical for the findings in this study, demonstrates that the health records information structure differs widely from the clinically logical structure build by the doctor. Not a single obser-view gave rise to an information structure with any resemblance to the health record's structure.
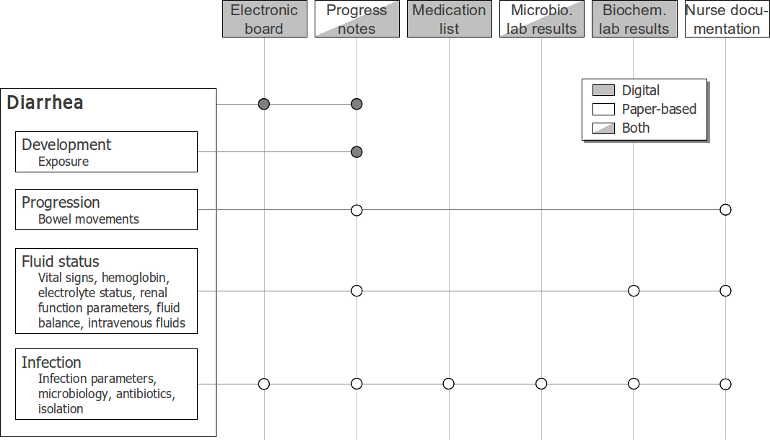
Figure 2. Example of how the health record's different source-sections contribute to the contextualization of topics. Same case as in Figure 1. Filled bullets mean: information from this source-section is exhaustive, empty bullets mean: information must be gathered from further source-sections.
3. Discussion
3.1. Experience With Methods Used
The obser-view method makes it possible to perceive the doctor's performance as a coherent sequence of focal points. It must be noted, though, that the perception of coherence depends on the observer's domain knowledge. Hence, the observer should be medically educated. The obser-view delays clinical work, but even though it poses a distinctly deviation from the ordinary work, it is also very similar to the way that doctors and medical students are taught, and thus it represents a situation which feels natural to the participant. The emphasis on dialog makes the method more susceptible to bias than the less relaxed thinking-aloud methods, partly because the observer through the dialogue may influence the doctor unintentionally, partly because the observer, as a result of medical education, may be blind to details of the doctor's behavior. The method of assembling the focal points into an information structure is also susceptible to bias: While most grouping and structuring of the focal points is given through the dialogue, some remains. To minimize bias regarding this, the assembling could be done by more than one researcher.
The methods used seem to be well suited to register and describe clinically logical information structure. However, steps should be taken to minimize observer-bias.
3.2. Does Information Structure Matter?
In general, the participating doctors contextualized the clinical information based on a consecutive use of the source-sections. This might be the result of professional tradition, and it certainly appears rational in a time-oriented perspective, as shifts between digital sections gave rise to idle time and stress. However, in a quality- or security-oriented perspective, this approach seems suboptimal: As shown in Figure 2, several topics are scattered over the health record. Thus, in order to make an exhaustive contextualization of such topics the doctor is forced to either switch between source-sections, or postpone parts of the contextualization until relevant source-sections have been processed. In either case, the doctor is subjected to split-attention, which is known to increase mental load[11] and increase the risk of medical errors[12]. Accordingly, doctors in the present study were a few times observed to actually forget topics.
It was not the aim of this study to compare clinically logical information structures across patients and doctors, but the material suggests that there is a significant accordance within focal points like e.g. ventilation, cardiac arrhythmia, infection, fluid status. This will be the subject of further studies, as "views" based on clinically logical information structure (e.g. an infection view, a fluid status view) could be central to development of health records with a better information structure.
4. Conclusion
Video-supported obser-view seems to be an adequate method to register the topics involved in a doctor's contextualization of clinical information and to uncover the resulting clinically logical information structure. The study demonstrates that the current health record’s information structure differs widely from the doctors’ clinically logical information structures. This difference is perceived as undesirable as it increases mental load and the risk of medical errors. It is concluded that the present health record is suboptimal. It is recommended to investigate whether "views" based on clinically logical information structure can facilitate doctors' retrieval of information.