Gert Galster, MD MI
Department of Health Science and Technology, Aalborg University, Aalborg, Denmark
Abstract
Reuse of clinical information plays a key role in the vision of a health sector with comprehensive semantic and pragmatic interoperability. Several papers have dealt with the secondary reuse of information, e.g. for statistics or research, while the primary reuse - clinical information reused in a clinical setting - has received less attention. On the basis of a qualitative literature review, this paper creates a categorised overview of the different causes to refrain from reuse of clinical information in clinical settings. The categorisation contributes to a greater understanding of failing reuse of clinical information in clinical settings, and it can probably be used in designing, evaluating and optimising clinical information systems. Further, it is speculated that the categorisation can be used in the process of identifying the concepts that constitute the context of clinical information.
Keywords
Clinical Informatics, Interoperability, Information reuse, Double documentation, Context
Introduction
In the Semantic Health Report[1], Stroetmann, Kalra et al. has outlined several degrees of interoperability. The most extensive shows a vision in which health-related information can be shared seamlessly across national boundaries, clinical information can be exchanged and reused for both clinical and non-clinical purposes, and any health actor can understand and integrate the information, as if it was generated locally.
This vision, which would be beneficial to patients, health care providers, and society as a whole, is far from being realised. Several papers - e.g. [2-4] - describe a characteristic consequence of the lack of interoperability, namely double documentation, where clinical information is duplicated instead of being reused.
In an earlier work on double documentation and the need for contextual information [5] it became obvious that in a clinical setting there can be several reasons to refrain from reusing information, although it apparently exists. Some reasons will lead to double documentation while others will lead to repeated examinations and samplings.
The Semantic Health Report[1] indicates various underlying causes of significance to interoperability, e.g. technical, political, organisational, and legal. In order to increase reuse of clinical information it may be of interest to view these causes in a clinical perspective. Thus, the objective of this paper is to identify and categorise the immediate causes to refrain from reuse of clinical information in clinical settings.
The method section describes how the literature was reviewed, and how the analysis was conducted. The result section categorises the different reasons to refrain from reuse of clinical information, including examples from each category. Finally, in the discussion section, the usage of the categorisation is discussed.
Methods
The topic of the present paper is the exploration of causes not to reuse clinical information. While some causes, like poor standardisation, are obvious and have achieved wide publicity, other reasons are more sporadically described. It has been of interest to provide a categorisation of the reasons to refrain from reuse, even though the information apparently exists.
Basis for the literature search was:
- An all-fields PubMed-search for "double documentation", "double registration", "dual documentation" OR "dual registration" (21 hits)
- An all-fields PubMed-search for "reuse*" AND ("clinical information" OR "clinical data") (54 hits)
- A GoogleScholar search for "reuse of clinical information" (29 hits)
- A GoogleScholar search for "reuse of clinical data" (44 hits)
The raw search did provide 139 papers. Challenges associated with reuse of clinical information was only mentioned in 26 papers, and only 15 did so related to reuse in clinical settings. It was therefore decided to extend the search through snowballing, and to supplement further with papers known to deal with double documentation and non-reuse of clinical information in clinical settings. In this way a total of 46 papers was included in the review. A complete list can be found at the authors homepage: http://gert.galster.dk/docs/20120826_MIE/.
The qualitative literature review was conducted, supported by the following question: "Is there any indication that existing clinical information is not reused, e.g. double documentation or repeated examinations and samplings. If so, for what reasons?".
It was possible to categorise the found causes along different lines. The actual categorisation was chosen partly because it is thought to be usable in designing, evaluating and optimising of clinical information systems, and partly because it is considered suitable as a basis for dialog with health workers about their need for contextual information.
Results
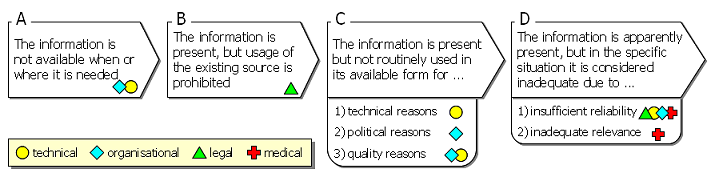
The literature review uncovered several reasons to refrain from reuse of clinical information. The described reasons can overall be categorised as follows: The information is …
- A) not available when or where it is needed
- B) present, but usage of the existing source is prohibited
- C) present but not routinely used in its available form
- D) apparently present, but in the specific situation it is considered inadequate
This structuring of causes corresponds to the situation, that a specific piece of information is needed (e.g. a diagnosis, a prescription, the result of an examination), and apparently it already exists. The issue of reuse depends on a progressive number of questions: Is the information available here and now? Is it permitted to use the information? Is there a general reason not to use this kind of information? Is there a situational reason?
A) The information is not available when or where it is needed
This includes e.g. absent paper records and inappropriately placed workstations. [4,6]
B) The information is present, but usage of the existing source is prohibited
This includes situations, where health personnel do not have proper authorization to access registries, or where the patient's informed consent is required but missing. [7,8]
C) The information is present but not routinely used in its available form
This category includes three quite different types of reason to refrain from reuse of clinical information: 1) technical, 2) political, and 3) quality reasons.
Technical reasons have achieved wide publicity, e.g. [1,2,4,9,10]. The basic problem is poor or non-existent interoperability between information systems ,e.g. paper-based versus electronic systems, and the usual consequence is either to copy/convert the information manually, or procure the information again.
By 'political reasons' is here referred to the rarely described phenomenon, that the different groups of health workers - e.g. physicians, nurses, midwives - each have a need to demonstrate and make visible their activities in order to manifest their authority and eligibility. [11-13]
As described in several papers, the achievement of sufficient data quality for systematic reuse is a challenge - not the least so in national or other major health registries. [1,3] Even if utilisation of such registries, as a source of reusable health information, would be very convenient, the lack of data quality may constitute a limiting factor. [5]
D) The information is apparently present, but in the specific situation it is considered inadequate
This category includes two distinct types of reason to refrain from reuse of clinical information: 1) insufficient reliability, and 2) inadequate relevance.
Some situations demand particularly reliable information [8,14], e.g. ensuring patient identity before surgery or obtaining consent for abortion.
But even under normal circumstances, failing credibility can justify, that clinical information is not (re)used; either because the information in its context is unreliable [3,9] - e.g. heart rate 800 bpm or a female with prostatism - or because the source of information is dubious. [15,16]
And even if the clinical information is perfectly reliable, it may be of inadequate relevance in the specific situation, either because the information lacks precision [3,17] or because its primary context makes it irrelevant in the specific situation. [5,15,18]
Examples of failing precision could be blood pressure listed as "elevated" or blood glucose without information about fasting.
Examples of failing relevance due to primary context could be the situations, where information gathered for one purpose cannot be reused for another purpose, e.g. clinical monitoring versus thorough examination. Other examples are the many situations, where "information shelf life" is significant, e.g. the body temperature from yesterday cannot be reused today (body temperature has a shelf life), and the septic patient's body temperature an hour ago cannot be reused now (diagnosis affects shelf life).
Discussion
In this work, the different causes to refrain from reuse of clinical information are seen from a clinical perspective. It should be noted that the main part of clinical information is gathered for clinical purposes and for (re)use in a clinical setting.
The clinical perspective makes it obvious, that even in the face of maximum reuse of clinical information and total interoperability, there will always be clinical information, that - on medical grounds - will not, and should not, be reused.
To examine causalities, like why information is not reused, is to open Pandora's box: there is always a reason for a reason, always another layer of causes. This work identifies some immediate causes to refrain from reuse of information, while the Semantic Health Report[1] indicates some underlying aspects of importance to interoperability. Figure 1 shows an attempt to link the immediate causes to their underlying aspects.
The present categorisation is intended as a help for understanding, why clinical information is not reused in clinical settings, even if it seems obvious to do so. Further, it should be possible to use the categorisation as an aid for designing and evaluating clinical information systems, in order to optimise the reuse of clinical information. The present structuring of causes is based on just this usage.
But the primary reason for this work was to develop a key to analyse the importance of different kinds of contextual information in clinical settings: Lack of contextual information has been stated as a significant reason for failing interoperability [15,17]. As stated by Bricon-Souf et al. [19], there is no consensus as to the best way to model context. A first step toward modeling is the uncovering of the underlying concepts. In continuation of the previous work on double documentation and the need for contextual information [5], it is of interest
- to assess the extent to which context is part of the decision whether to reuse clinical information, and
- to identify the concepts that constitute clinical information's context.
The list of causes to refrain from reuse of clinical information makes it possible to relate the significance of context to these causes. It turns out that if the information is available (B, C, D), then context plays a decisive role in every of the listed causes, e.g. source of information (B, C2, C3, D1), timing of information (B, D), primary documentation system (C1, C3, D1), and a variety of clinical contextual information (D). It is speculated that this approach can help to identify the concepts that constitute the context of clinical information. Application of the present categorisation will be included as part of a future work with this purpose.
It is concluded that the present categorisation contributes to a greater understanding of failing reuse of clinical information in clinical settings. It is expected that the categorisation can be used in designing, evaluating and optimising clinical information systems. It is speculated that the categorisation can be used in the process of identifying the concepts that constitute the context of clinical information.